What does it take to prevent malaria? Some of the programs GiveWell recommends might sound straightforward—for example, seasonal malaria chemoprevention (SMC) programs provide antimalarial drugs to young children—but the process of accomplishing this is not simple at all.
Below, we offer a post from Malaria Consortium that describes the many complex steps required to carry out an SMC campaign. See our reports for more information about the evidence for SMC and about Malaria Consortium’s SMC program.
You can read the original post on Malaria Consortium’s website.
***
Distributing anti-malaria medicines to 25 million children: The supply chain step-by-step
Ashley Giles, Nkoli Nnamonu and Lawrence Ekeocha, August 16, 2023
Author’s note: This blog is an update from the original article published in 2019. Since then, Malaria Consortium’s SMC activities have grown from targeting six million children to 25 million children in 2023. This expansion has taken place as a result of geographic expansion to new areas of Nigeria, in addition to SMC implementation research in Mozambique, South Sudan and Uganda. The work continues to take place in close collaboration with national malaria programmes and generous support from philanthropists and institutional donors.
The moment a community distributor gives a spoonful of life-saving malaria medicine to each of 25 million children across sub-Saharan Africa this year, it marks the finish line of a long and winding road from manufacturer to community.
Since 2013, Malaria Consortium has supported the transportation and distribution of medicines for seasonal malaria chemoprevention (SMC), an intervention recommended by the World Health Organization (WHO), in areas where malaria transmission peaks during the rainy season. SMC involves the distribution of full courses of safe and effective antimalarial medication (a combination of two drugs, sulfadoxine-pyrimethamine (SP) and amodiaquine (AQ) in four monthly intervals, or five in some regions, during the rainy season to those most at risk: children under five. The aim is to maintain sufficient levels of antimalarial drugs in children’s bloodstreams throughout the period when malaria transmission is at its highest. SMC, which has been implemented in areas of West Africa since 2013, has now expanded to include communities in parts of East and southern Africa. In 2022, Malaria Consortium reached children in seven countries: Burkina Faso, Chad, Mozambique, Nigeria, South Sudan, Togo and Uganda.

So how do the drugs reach the children who need them? Our operations team oversees this process; from calculating the numbers of drugs needed through to overseeing their distribution to the health facilities. From there, the drugs are dispensed with the support of the programmes team. Preparations for the campaign involves six steps, from ordering the drugs to passing them to distributors.
Step one: Ordering and manufacturing the drugs
The drugs required are in high demand globally and there are only three manufacturers that are pre-approved by WHO to produce them, with two of these manufacturers based in India and one in China. When this factor is added to the number of blister strips of drugs needed for our campaign – around 78 million – there is no alternative: we must order the drugs we need at least one year before the distribution campaign begins following a quantification process conducted in collaboration with national malaria programmes to estimate the numbers of medicines needed. Each blister strip contains the medicines needed for a full course of SPAQ: one tablet of SP and three tablets of AQ.
Once the drugs have been produced, the baton is passed to third-party international freight forwarders for the next stage of the process.
Step two: Transporting the medicines across oceans and continents
From the factory near Guilin in China, or those in Gujarat and Mumbai in India, SMC medicines begin a journey of tens of thousands of kilometres, passing overland from ports in Shanghai, or Nhava Sheva, crossing the Indian Ocean to reach the African continent. Following good distribution practice, medicines to be distributed via sea freight are transported in generator-powered refrigerated containers, also called reefers, to keep them at optimum temperature and humidity, thus ensuring stability of medicines while in transit. Data loggers in the reefers provide updates on temperature and humidity whenever a ship comes close to land, as well as at the destination port. Temperature-controlled solutions for air freight include cool dollies and thermal blankets. It is important for commodities to remain in the same container during transit to maintain the recommended temperature and humidity conditions set prior to shipment.
Step three: SMC medicines arrive at ports around Africa
Malaria Consortium’s Commodity and Logistics Managers can track all shipments using a tracker dashboard before the drugs arrive at seaports and airports in Lagos, Abuja, or Port Harcourt (Nigeria), Douala (Cameroon), Mombasa (Kenya), Juba (South Sudan), Beira (Mozambique), and Lome (Togo). Once the shipments arrive at the ports, the longest stretch of the medicines’ journey is complete, but there are still several hurdles to overcome. For Burkina Faso, Chad and Uganda, freight is transported overland to Ouagadougou, N’Djamena, and Kampala, dealing with border crossings en route. The Operations team in each country is then responsible for ensuring the medicines move through customs and on to the respective central medical stores.
Step four: Quality control
Central medical stores hold the commodities for quality control and testing. At this stage, Malaria Consortium’s Operations team carries out a stock reconciliation to ensure the correct quantity of medicines has been received at the stores, and that the quality seals on the packaging are inspected. In some countries, the commodities are quarantined on arrival and checked by authorities. For others, the drugs control authority inspects the shipments before departure at country of origin to ensure the medicines are legitimate and that valid licences are held by the recipients.
Once this process is complete, the medicines can be sent to local laboratories, where samples are tested to ensure their quality after the long journey. After quality assurance tests are passed, medicines are deemed safe for distribution.
Step five: From the store to the districts
The local Operations team’s final task in each country is to ensure the medicines reach the states or districts where SMC is implemented. The teams work to ensure the correct quantity of commodities reach each district. Once the medicines are in the area where they are due to be distributed from, they are put into storage for one to three months ahead of the campaign starting. This also gives the team the chance to do final stock reconciliation and ‘kitting’ the medicines per health facility requirements for each cycle – which can take days, as some states can be dealing with millions of blister strips per cycle. Kitting involves arranging medicines with items that facilitate administration, such as, plastic cups, spoons, aprons, hand gloves, etc., sourced separately in each country. After this, the responsibility for the commodities is handed over to Malaria Consortium’s programme team and around 180,000 community distributors, who take over the baton from there.
Step six: Reaching 25 million children
Distribution of the SMC drugs takes place door-to-door across Burkina Faso, Chad, Mozambique, Nigeria, South Sudan, Togo, and Uganda to coincide with the rainy seasons in these regions. Alongside the logistical efforts to ensure the drugs are available in time for the beginning of the distribution campaigns, Malaria Consortium has also been helping to train community distributors and their supervisors to dispense drugs to eligible children and to ensure that the treatments are given according to guidelines.
The SMC campaign is delivered in ‘cycles’ – a four-day period every month for four months (or five months in some regions) according to the rainfall in each location. A few days before each cycle a huge exercise is undertaken by the Operations team and the local Ministry of Health stock managers to move the commodity kits to thousands of health facilities across the seven countries. At the start of each cycle, the child’s caregiver receives a blister strip of the SMC drugs from the community distributors and the first doses of SP and AQ are taken when the distributor is present so they can learn how to administer the drugs. The caregiver then gives the child the two remaining doses of AQ over the next two days. Malaria Consortium and partners have worked with the manufacturer to create a tablet that dissolves in water and is sweetened to be more acceptable to the child.
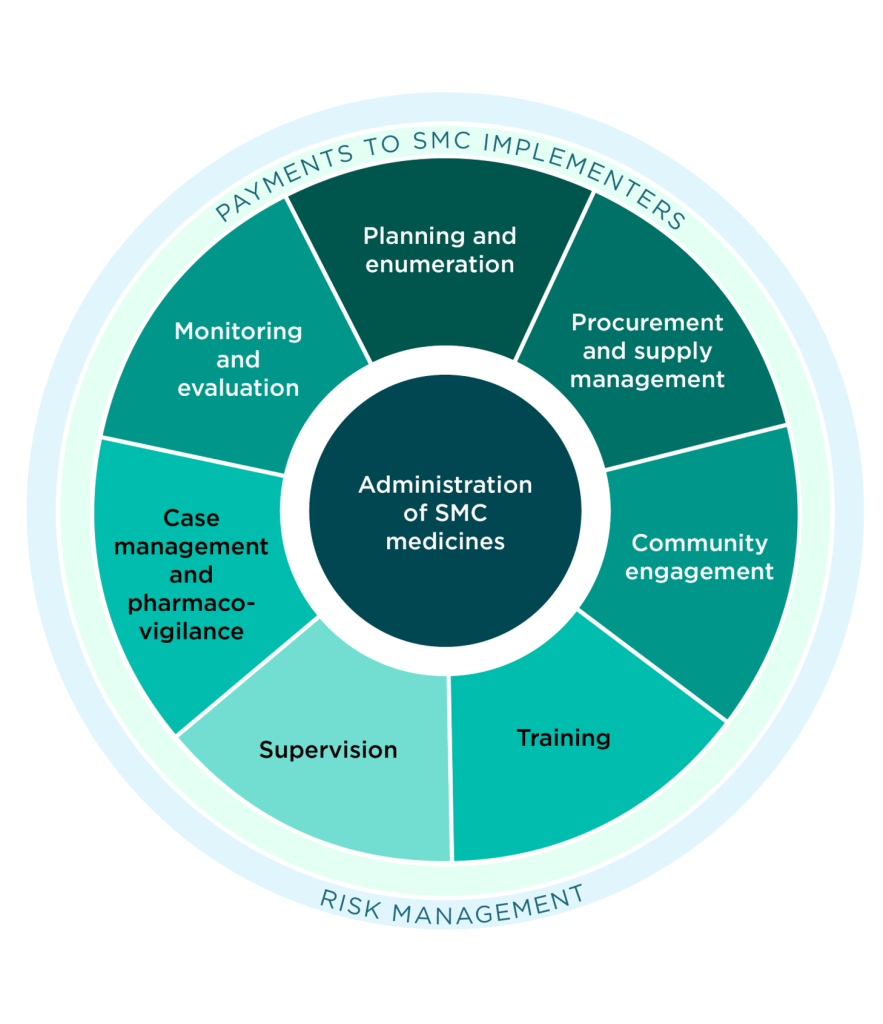
The SMC procurement and supply management is one of nine key components that form the SMC administration process, this takes place alongside Malaria Consortium’s SMC research strategy which is helping to plot the future of the intervention. In 2023, we are targeting around 25 million children with SMC across the seven countries. By the end of the year, 78 million blister packs of SMC medicines will have completed their journey from Guilin, Gujarat, and Mumbai via a multitude of customs and quality checks, and transit through each country, to bloodstreams of the children most vulnerable to malaria infection, protecting them from disease.
