This post is the second in a multi-part series, covering how GiveWell works and what we fund. Through these posts, we hope to give a better understanding of our research and decision-making. Links to the other posts:
- How we work, #1: Cost-effectiveness is generally the most important factor in our recommendations
- How we work, #3: Our analyses involve judgment calls
- What we fund, #1: We fund many opportunities outside our top charities
Looking forward, not just backward
When we consider recommending funding, we don’t just want to know whether a program has generally been cost-effective in the past—we want to know how additional funding would be used.
People sometimes think of GiveWell as recommending entire programs or organizations. This was more accurate in GiveWell’s early days, but now we tend to narrow in on specific opportunities. Rather than asking whether it is cost-effective to deliver long-lasting insecticide-treated nets in general, we ask more specific questions, such as whether it is cost-effective to fund net distributions in 2023 in the Nigerian states of Benue, Plateau, and Zamfara, given the local burden of malaria and the costs of delivering nets in those states.
Geographic factors affecting cost-effectiveness
The same program can vary widely in cost-effectiveness across locations. The burden of a disease in a particular place is often a key factor in determining overall cost-effectiveness. All else equal, it’s much more impactful to deliver vitamin A supplements in areas with high rates of vitamin A deficiency than in areas where almost everyone consumes sufficient vitamin A as part of their diet. Similarly, one of our top charities, New Incentives, has chosen to operate in northern Nigeria largely because relatively low baseline vaccination rates mean its work is especially impactful there.[1]
As another example, we estimate it costs roughly the same amount for the Against Malaria Foundation to deliver an insecticide-treated net in Chad as it does in Guinea (about $4 in both locations). But, we estimate that malaria-attributable deaths of young children in the absence of nets would be roughly 5 times higher in Guinea than in Chad (roughly 8.8 deaths per 1,000 per year versus roughly 1.7 per 1,000), which leads AMF’s program to be much more cost-effective in Guinea. Overall, we estimate that AMF’s program is around 27x cash in Guinea and around 5x cash in Chad.[2]
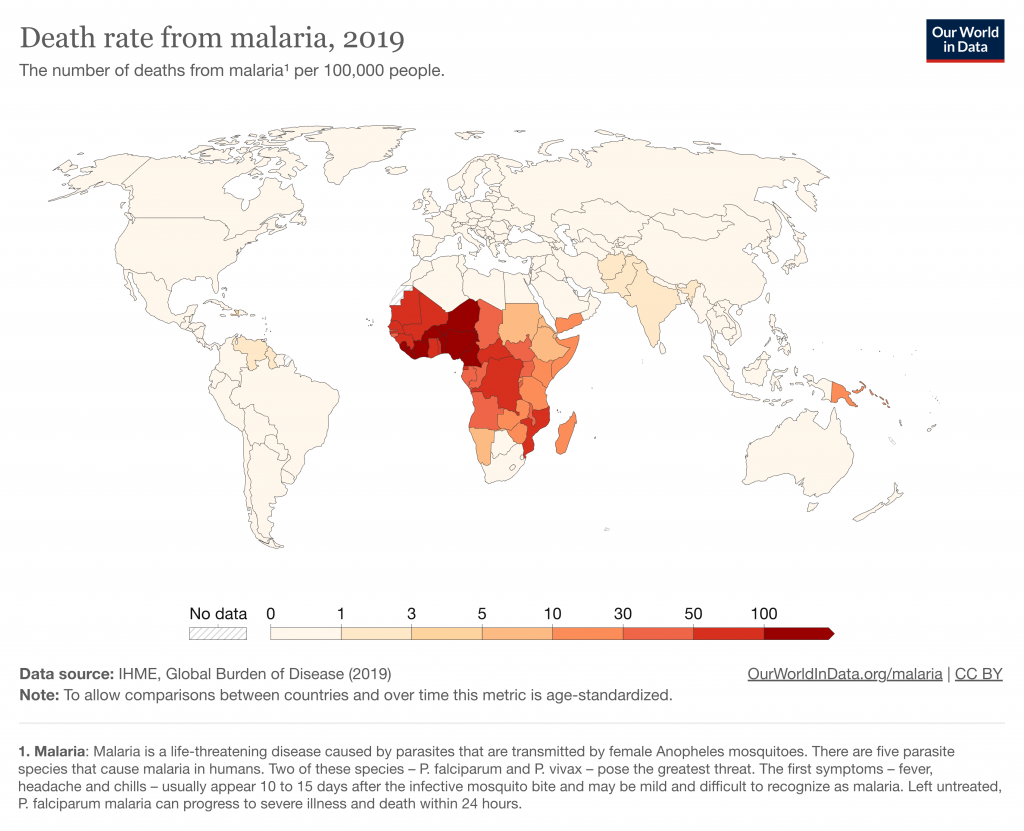
This map from Our World in Data gives a sense of how deaths from malaria vary worldwide.[3]
Because cost-effectiveness varies with geography, we ask questions specific to the countries or regions where a program would take place. When we were investigating an opportunity to fund water chlorination in Malawi, for example, we wanted to know:
- How does baseline mortality from poor water quality in Malawi compare with that in the regions where the key studies on water chlorination took place?
- What is the overall morbidity burden from diarrhea in Malawi?
- Might people be more or less likely to use chlorinated water in this area than in the areas where the key studies took place?
- What does it cost to serve one person with in-line chlorination for one year? We calculate this, in part, by estimating how many people are served by each device.
- What proportion of the population is under the age of five? This is important to our calculations because we think young children are disproportionately susceptible to death from diarrhea.
- What is the baseline level of water treatment in the absence of this program?
Where relevant, we also consider implementation challenges caused by security concerns or other contextual factors.
Why do cost-effective funding gaps sometimes go unfilled?
People are often surprised that some high-impact funding gaps, like the ones GiveWell aims to fund, aren’t already filled. Of course, many high-impact opportunities are already supported by other funders, like Gavi or the Global Fund, to name just a couple examples. When we see remaining gaps, we think about how our grant might affect other funders’ decisions, and whether another funder would step in to fill a particular gap if we didn’t.[4]
The priorities of major funders and their funding guidelines can lead to some gaps going unfilled despite urgent needs. For example, the Global Fund (the major multilateral funder of programs addressing malaria, tuberculosis, and HIV/AIDS) caps the malaria support any individual country can receive at 10% of the Global Fund’s total malaria funding. Nigeria has more than one-quarter of the global burden of malaria, and the cost to address that burden far exceeds 10% of the Global Fund’s malaria funding. As a result, there are often unfilled, cost-effective gaps for programs like nets and seasonal malaria chemoprevention (SMC) in Nigeria.[5]
Putting your donations to good use
When we recommend grants (as we do when donors give to the All Grants Fund or the Top Charities Fund, or when we recommend opportunities to individual large donors like Open Philanthropy), we look at the specific country or subnational region where funding might be used, and estimate the cost-effectiveness of the location-intervention pair (e.g., SMC in Burkina Faso or deworming in Chad). Generally, if the location-intervention pair seems to be above our cost-effectiveness bar (as discussed in the first post in this series), we recommend a grant.[6]
We focus on the specific context in which funds will be used for the full range of programs we consider, whether they are programs directly delivering goods (e.g., providing vitamin A supplementation), technical assistance programs (e.g., supporting syphilis testing and treatment during pregnancy), academic research (e.g., studying water chlorination), or pilots of new programs (e.g., delivering perennial malaria chemoprevention in the Democratic Republic of the Congo). In future posts, we’ll share more about the variety of programs we support.
When you give to our top charities, you can trust that they can use additional funding productively (see our criteria for top charities). And when you give to the All Grants Fund (our top recommendation) or the Top Charities Fund, you benefit from our research to ensure that your donation goes to the most pressing, cost-effective funding gaps we’re aware of at the time.[7]

Comments
Is it worth trying to persuade the Global Fund to raise or eliminate its per-country cap on expenditure? I’m sure they have their reasons, but perhaps there’s room to persuade them that having the cap at say 15% might enable them to save or improve many more lives.
Hi Ben,
Thanks for raising this question!
We’ve thought about this idea in our past work on policy advocacy and aid effectiveness. Because we think that the cost-effectiveness of the malaria interventions the Global Fund supports varies significantly by the disease burden in each country, we believe raising or eliminating its spending caps would increase the overall cost effectiveness of its funding for these programs.
That said, we’re unsure if we’ll prioritize exploring opportunities to influence this in the future. Experts we’ve talked to have generally been skeptical about the feasibility of influencing the Global Fund to raise its spending caps—and we would be cautious of potential adverse outcomes (for example, if changing its spending caps would make it harder for the Global Fund to fundraise from its primary donors). Given the potential benefit, though, we plan to continue seeking outside input, and we might revisit this (and other funding advocacy opportunities) as we build staff capacity and expertise.
I hope this is helpful! Please let me know if you have any other questions.
All the best,
Roman
Comments are closed.